Urgent care centers play a vital role in the U.S. healthcare system by delivering fast, affordable, and accessible medical services. However, behind the speed of patient care lies a complex administrative function that directly impacts financial stability—urgent care billings. Accurate billing is essential not only for timely reimbursements but also for maintaining compliance, reducing denials, and sustaining long-term growth.
As urgent care facilities continue to expand across the USA, understanding the nuances of billing and coding has become more important than ever. This guide explores how urgent care billing works, common challenges, and best practices to ensure clean claims and optimized revenue.
What You’ll Learn in This Blog
-
How urgent care billings differ from other medical billing models
-
Key components that affect reimbursement accuracy
-
Common billing challenges faced by urgent care centers
-
Best practices to improve claim acceptance rates
-
How professional billing support can streamline operations
Understanding Urgent Care Billings
Urgent care billings refer to the process of translating patient visits, treatments, and services into accurate insurance claims for reimbursement. Unlike traditional physician offices or emergency departments, urgent care centers operate with high patient volumes, extended hours, and a wide range of services—all of which add complexity to billing workflows.
Urgent care visits often include:
-
Evaluation and management services
-
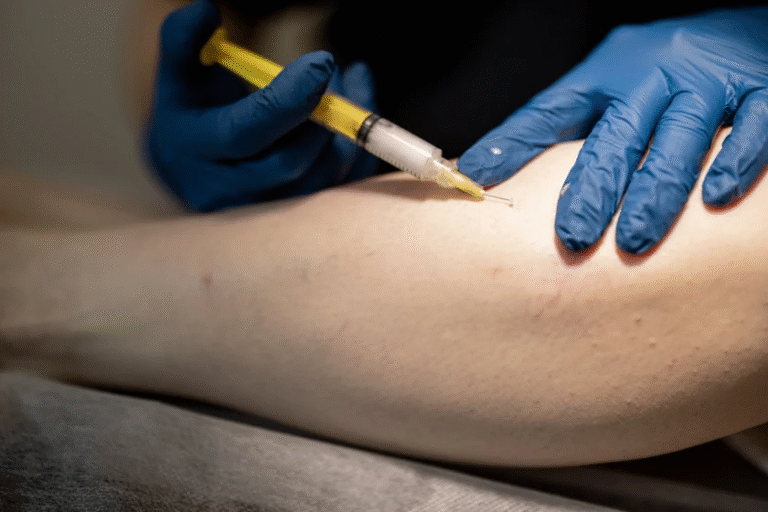
Minor procedures and wound care
-
Diagnostic tests and imaging
-
Vaccinations and occupational health services
Each service requires precise documentation, correct coding, and payer-specific claim submission rules.
Why Urgent Care Billing Is Uniquely Challenging
Urgent care billing sits at the intersection of primary care and emergency medicine. This creates operational challenges that require specialized billing knowledge.
High Patient Volume
Urgent care centers often see dozens or even hundreds of patients per day. Managing this volume while ensuring documentation accuracy can be difficult without structured billing processes.
Diverse Payer Mix
Urgent care facilities bill Medicare, Medicaid, commercial insurers, workers’ compensation, and self-pay patients. Each payer has different coverage rules, reimbursement rates, and filing requirements.
Same-Day Coding Complexity
Services provided during urgent care visits frequently involve multiple procedures. Coding errors, missing modifiers, or incorrect levels of service can easily lead to claim denials.
Core Components of Effective Urgent Care Billings
Accurate Patient Registration
Billing success begins at the front desk. Collecting correct patient demographics, insurance details, and eligibility verification helps prevent downstream claim rejections.
Detailed Clinical Documentation
Providers must clearly document the reason for visit, medical decision-making, procedures performed, and time spent. Incomplete or vague notes are a major cause of billing errors.
Correct CPT and ICD-10 Coding
Coding must accurately reflect the services provided. Overcoding or undercoding can both result in compliance risks or revenue loss.
Timely Claim Submission
Urgent care billings require fast turnaround times. Delayed submissions can exceed payer filing limits and reduce reimbursement potential.
Common Billing Errors in Urgent Care Centers
Even experienced practices encounter billing challenges. Some of the most frequent issues include:
-
Incorrect evaluation and management level selection
-
Missing or invalid modifiers
-
Inconsistent diagnosis-to-procedure linking
-
Duplicate claim submissions
-
Lack of documentation to support billed services
Addressing these issues proactively can significantly reduce denial rates and improve cash flow.
The Role of Compliance in Urgent Care Billings
Compliance is a critical aspect of billing operations. Urgent care centers must adhere to federal and state regulations, payer guidelines, and coding updates. Failure to comply can result in audits, penalties, or revenue recoupment.
Key compliance areas include:
-
Proper use of modifiers
-
Adherence to medical necessity requirements
-
Accurate reporting of services performed
-
Regular updates to coding and billing protocols
Maintaining compliance requires continuous education and consistent internal audits.
Best Practices to Improve Urgent Care Billing Performance
Implement Standardized Workflows
Standard operating procedures help staff follow consistent billing steps, reducing variability and errors.
Invest in Staff Training
Regular training ensures billing and coding teams stay updated with payer changes and coding revisions.
Monitor Key Billing Metrics
Tracking denial rates, days in accounts receivable, and clean claim ratios helps identify problem areas early.
Leverage Technology Wisely
Billing software and practice management systems can automate eligibility checks, coding validation, and claim tracking.
Outsourcing Urgent Care Billings: A Strategic Advantage
Many urgent care providers choose to outsource billing to specialized partners to improve efficiency and reduce administrative burden. Professional billing services bring industry expertise, dedicated resources, and scalable solutions.
247 medical billing services supports urgent care centers across the USA by delivering customized billing solutions designed to maximize reimbursements while maintaining full compliance. With experienced billing professionals and robust quality checks, urgent care practices can focus more on patient care and less on paperwork.
Financial Impact of Optimized Billing Processes
When urgent care billings are managed correctly, the financial benefits are measurable:
-
Faster reimbursement cycles
-
Reduced claim denials
-
Improved cash flow stability
-
Better visibility into revenue performance
-
Enhanced patient satisfaction through transparent billing
Optimized billing directly contributes to operational sustainability and long-term growth.
Future Trends in Urgent Care Billing
The urgent care landscape continues to evolve with changing payer models, value-based care initiatives, and increased regulatory oversight. Billing processes must adapt to:
-
Telemedicine and hybrid care models
-
Real-time eligibility and price transparency
-
Increased emphasis on documentation quality
-
Data-driven revenue cycle management
Staying ahead of these trends ensures billing operations remain resilient and compliant.
Conclusion
Urgent care billings are far more than an administrative task—they are the financial backbone of urgent care operations. From accurate documentation and coding to compliance and payer communication, every step plays a role in revenue integrity. By implementing best practices and partnering with experienced billing professionals like 247 medical billing services, urgent care centers in the USA can achieve consistent reimbursements, reduce denials, and focus on delivering timely, high-quality care.
Frequently Asked Questions
What makes urgent care billing different from other medical billing?
Urgent care billing involves high patient volumes, diverse services, and multiple payer types, requiring specialized workflows and coding expertise.
How can urgent care centers reduce claim denials?
Accurate documentation, correct coding, eligibility verification, and timely claim submission are key to minimizing denials.
Is outsourcing urgent care billing cost-effective?
Yes. Outsourcing often reduces administrative overhead, improves claim accuracy, and accelerates reimbursement timelines.
How often should billing audits be conducted?
Regular internal or external audits should be conducted at least quarterly to ensure compliance and identify revenue leakage.
Can professional billing services improve cash flow?
Absolutely. Experienced billing partners streamline processes, reduce errors, and improve overall revenue cycle performance.